
Medical and Endoscopic management of various chronic conditions.

Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) is a urological condition characterized by persistent pain and discomfort in the pelvic region, often accompanied by urinary symptoms. Unlike acute bacterial prostatitis, CP/CPPS does not typically involve an active bacterial infection. This condition is the most common type of prostatitis and can be challenging to diagnose and manage.
CP/CPPS is categorized into two types: inflammatory (Type IIIA) and non-inflammatory (Type IIIB). Inflammatory CP/CPPS is associated with inflammation and immune system activation in the prostate, while non-inflammatory CP/CPPS is not.
The primary symptoms of CP/CPPS include pelvic pain or discomfort, pain in the genital area, lower back pain, and urinary symptoms like urinary urgency, frequency, and discomfort. The exact cause of CP/CPPS remains unclear, but it may involve a combination of factors, including infection, inflammation, neuromuscular abnormalities, and psychological factors.
Treatment approaches for CP/CPPS typically include a combination of lifestyle modifications, physical therapy, and medications. This may involve pain management, muscle relaxation techniques, and, in some cases, the use of alpha-blockers or anti-inflammatory medications. Psychological counseling and stress management techniques can also be beneficial for some patients.
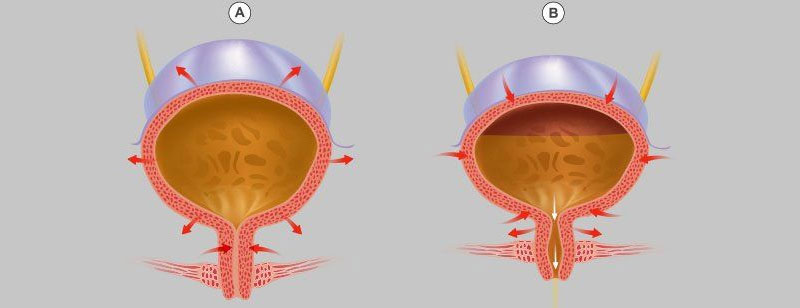
Overactive bladder (OAB) is a common and often distressing urological condition characterized by a variety of urinary symptoms, primarily urinary urgency, frequency, and sometimes incontinence. OAB results from abnormal bladder muscle contractions, causing the bladder to contract involuntarily, leading to these bothersome symptoms.
OAB can significantly impact a person's quality of life, causing embarrassment, anxiety, and affecting daily activities. The exact cause of OAB is not always clear and can result from a combination of factors, including age, neurological conditions, urinary tract infections, or medications.
Management of OAB typically involves lifestyle modifications, bladder training exercises, and, in some cases, medications such as anticholinergics or beta-3 agonists, which help relax the bladder and reduce the symptoms. Behavioral therapies and pelvic floor exercises can also be beneficial.
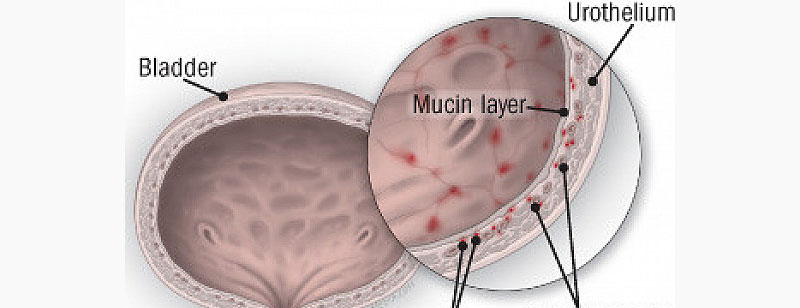
Interstitial cystitis (IC), also known as painful bladder syndrome, is a chronic and often debilitating urological condition characterized by pain and discomfort in the bladder and pelvic region. This condition affects the bladder's lining and can lead to a range of urinary symptoms, making it a challenging and painful condition for those affected.
The exact cause of interstitial cystitis remains unclear, and it is often a diagnosis of exclusion, ruling out other potential causes of urinary symptoms. Researchers believe that a combination of factors, including inflammation, damage to the bladder lining, and abnormal immune responses, may contribute to the development of IC.